What Is Diabetic Retinopathy?
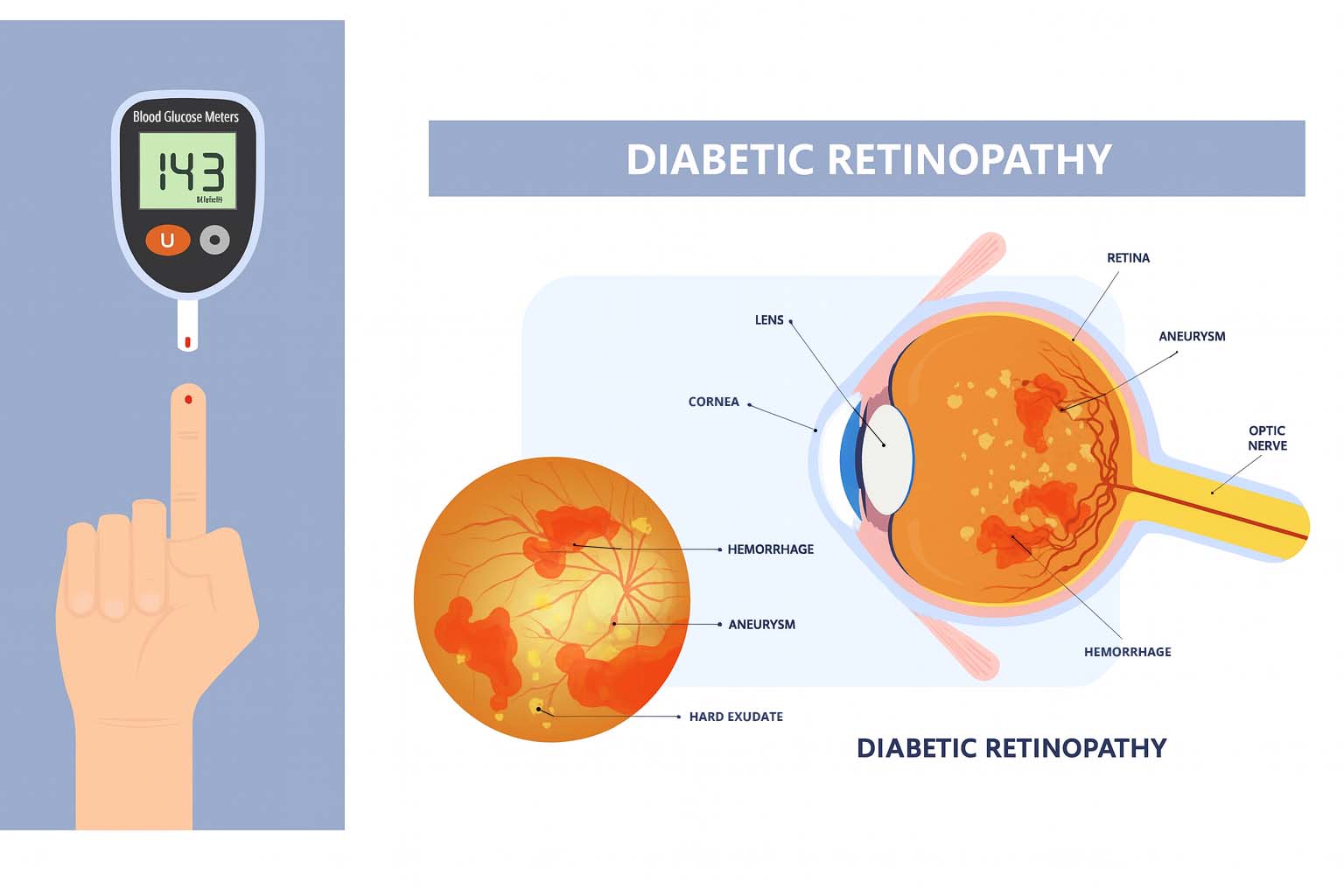
Diabetic retinopathy is a complication of diabetes that injures the retina’s tiny blood vessels. High blood sugar can make these vessels leak, swell, or close; in advanced stages, fragile new vessels can grow and bleed. Because the retina enables sharp, central vision, damage can make it harder to read, drive, or see fine detail. With early diagnosis and treatment, the risk of vision loss drops significantly.
Non-Proliferative vs. Proliferative
Non-Proliferative Diabetic Retinopathy (NPDR)
Non-Proliferative Diabetic Retinopathy (NPDR) is the early stage of diabetic eye disease. At this stage, small weak spots called microaneurysms form in the tiny blood vessels of the retina. These vessels may leak blood or fluid, causing swelling in the macula (the part of the eye responsible for sharp, central vision). Most people don’t notice any vision changes at this point, which is why regular dilated eye exams are so important for early detection.
Proliferative Diabetic Retinopathy (PDR)
Proliferative Diabetic Retinopathy (PDR) is the advanced stage of the disease, marked by the growth of abnormal new blood vessels in the retina. These fragile vessels can bleed into the eye, form scar tissue, and sometimes lead to retinal detachment, all of which significantly increase the risk of permanent vision loss.
Symptoms Patients May Notice
- Blurred or fluctuating vision
- Floaters or dark spots
- Trouble reading or recognizing faces
- Sudden vision loss if bleeding occurs
What Causes Retinal Vascular Diseases?
Retinal vascular diseases occur when blood flow to the retina is disrupted—by blocked arteries or veins, or by vessel wall damage. They are more common in people with diabetes, high blood pressure, or cardiovascular disease.
Retinal Vein Occlusion (BRVO/CRVO)
A blockage in a retinal vein prevents normal blood drainage and can cause swelling and hemorrhage.
- BRVO: A smaller branch vein is blocked, affecting part of the retina.
- CRVO: The main vein is blocked, often causing widespread swelling and vision loss.
Patients may notice blurry vision, dark spots, or a sudden decrease in sight.
Retinal Artery Occlusion (Eye Stroke)
A blockage in a retinal artery—often from a clot or plaque—cuts off oxygen to the retina and causes sudden, painless, severe vision loss in one eye. This is a medical emergency and may signal vascular disease elsewhere.
Hypertensive Retinopathy
Chronic high blood pressure damages retinal vessels, causing them to thicken, narrow, or leak. It often progresses silently but may eventually lead to blurred vision or bleeding.
How Are These Conditions Diagnosed?
Retina specialists use several quick, painless tests to detect disease—even before symptoms appear:
- Dilated Eye Exam: Pupil-widening drops allow a thorough view of the retina.
- Optical Coherence Tomography (OCT): Cross-sectional imaging shows swelling, fluid, and structural changes.
- Fluorescein Angiography: A dye highlights retinal vessels to reveal leaks, blockages, or abnormal growth.
- Fundus Photography: High-resolution photos track retinal changes over time.
Treatment Options
Treatment aims to halt progression, preserve vision, and often restore some sight. The best approach depends on the condition and severity.
Anti-VEGF Injections
Medications (e.g., Avastin®, Lucentis®, Eylea®) block VEGF, a protein that drives abnormal vessel growth and swelling. Injections reduce leakage, shrink abnormal vessels, and can improve vision. Treatments are typically repeated every 4–12 weeks.
Laser Therapy
Laser photocoagulation seals leaking vessels and shrinks abnormal growth. It is often used for proliferative diabetic retinopathy or to help control macular edema, and may be combined with injections.
Vitrectomy Surgery
For advanced bleeding or scar tissue, a vitrectomy removes the vitreous gel, clears blood, and relieves traction on the retina. In some cases, a gas bubble supports healing. This outpatient procedure helps stabilize or improve vision.
Living With Retinal Vascular Disease
Managing overall health is critical to protecting long-term vision. Follow your specialist’s plan and focus on healthy habits:
- Keep blood sugar under tight control if you have diabetes
- Manage blood pressure and cholesterol
- Exercise regularly and maintain a healthy diet
- Quit smoking to improve circulation
- Attend regular follow-up exams as advised
Vision changes can be stressful, but most patients maintain useful vision with consistent monitoring and timely treatment.
When to See a Retina Specialist
Seek care right away if you notice any of the following warning signs:
- Sudden vision loss in one or both eyes
- New floaters or flashes of light
- A dark curtain or shadow across your vision
- Rapidly worsening blurry vision
Even without symptoms, people with diabetes or vascular risk factors should have a comprehensive dilated eye exam at least once a year. Early treatment greatly improves the chances of protecting your vision.
Frequently Asked Questions
-
What are the first signs of diabetic retinopathy?
In the early stages, diabetic retinopathy may not cause any noticeable symptoms, which is why regular eye exams are so important. As the disease progresses, patients may begin to notice blurred or fluctuating vision, trouble reading fine print, or seeing dark spots and floaters in their vision. Some people describe straight lines appearing wavy or distorted. Because vision changes often happen gradually, it’s easy to ignore early warning signs. By the time vision loss becomes noticeable, the condition may already be advanced. The best way to protect your sight is to schedule yearly dilated eye exams if you have diabetes. Your eye doctor can detect diabetic retinopathy early with specialized imaging, long before you develop vision loss.
-
Can diabetic retinopathy cause blindness?
Yes, diabetic retinopathy is one of the leading causes of blindness in adults, especially if it is left untreated. The condition damages the retina’s delicate blood vessels, which can leak fluid, bleed into the eye, or cause scar tissue that distorts or detaches the retina. Over time, these changes can result in permanent vision loss. However, the good news is that with regular monitoring, timely diagnosis, and modern treatments such as injections, laser therapy, or surgery, most people with diabetic retinopathy can preserve useful vision. The key is early detection. If you have diabetes, strict control of blood sugar, blood pressure, and cholesterol also plays a major role in reducing your risk of serious complications.
-
What is an eye stroke, and how is it related to the retina?
NAn eye stroke is the layman’s term for a retinal artery occlusion, which happens when blood flow to the retina is suddenly blocked by a clot or cholesterol plaque. Because the retina requires a constant supply of oxygen, a blockage can cause sudden, painless, and severe vision loss in one eye. Unfortunately, once vision is lost from an eye stroke, it is often permanent. Retinal artery occlusions are also considered medical emergencies because they can signal vascular problems elsewhere in the body, such as a risk of stroke or heart attack. If you experience a sudden loss of vision in one eye, you should seek emergency medical care immediately. While treatment options are limited, urgent care can help protect your overall health and, in some cases, minimize permanent damage.
-
How are diabetic retinopathy and retinal vein occlusion treated?
Treatment depends on the severity of the disease. For diabetic retinopathy, common treatments include anti-VEGF injections, which block abnormal blood vessel growth and reduce swelling, and laser therapy to seal leaking vessels. In advanced cases with bleeding or scarring, vitrectomy surgery may be necessary. Retinal vein occlusion, which occurs when a vein is blocked, is also treated with anti-VEGF injections to reduce fluid buildup (macular edema) and laser therapy if needed. In all cases, controlling underlying conditions such as diabetes, high blood pressure, and cholesterol is just as important as eye-specific treatments. With today’s therapies, many patients can maintain or even improve their vision if treatment begins promptly.
-
Do injections for retinal disease hurt?
Many patients are understandably nervous about the idea of an injection in the eye, but the procedure is usually quick and virtually painless. Before the injection, your eye is numbed with anesthetic drops and thoroughly cleaned to prevent infection. Most patients report only mild pressure or a slight pinch, and the entire process often takes less than a minute. Afterward, you may notice mild irritation, tearing, or the sensation of something in your eye, but this typically resolves within a day or two. Your retina specialist will provide instructions on how to care for your eye after the injection. These injections are highly effective at reducing swelling, stopping abnormal blood vessel growth, and preserving vision, which makes the minor discomfort well worth the benefits.
-
How often should I get an eye exam if I have diabetes?
Most people with diabetes should have a comprehensive dilated eye exam at least once a year, even if their vision seems normal. If diabetic retinopathy is already present, your eye doctor may recommend exams more often—sometimes every 3–6 months—depending on the severity. Regular exams allow retina specialists to detect changes early, when treatment is most effective. Skipping exams is risky because diabetic retinopathy often progresses silently without noticeable symptoms in its early stages. In addition to eye exams, controlling your blood sugar, blood pressure, and cholesterol can significantly reduce the risk of vision complications. If you experience sudden changes such as floaters, dark spots, or sudden vision loss, schedule an appointment right away.
-
Is vision loss from diabetic retinopathy reversible?
Whether vision improves after treatment depends on the severity and duration of the disease. In many cases, treatments such as anti-VEGF injections or laser therapy can significantly reduce swelling and restore some clarity to vision, especially if started early. However, damage to the retina from long-standing disease may not be fully reversible. The goal of treatment is to prevent further loss, stabilize vision, and in many patients, improve sight enough to read, drive, and maintain independence. That’s why timely diagnosis and consistent follow-up are so important. With today’s advanced therapies, many people with diabetic retinopathy can continue to enjoy a good quality of life and functional vision well into the future.

Protect Your Vision Today
If you’re living with diabetes or vascular health risks, don’t wait for symptoms to appear. Early detection and treatment of retinal disease can prevent permanent vision loss and keep your sight clear for years to come.
Schedule Your Retinal Evaluation or give us a call at 208-535-4900
